作者简介:黄道政(1982-),男,海南三亚人,主治医师,硕士研究生,研究方向为老年危重患者的综合救治。
目的 研究老年念珠菌血症所致感染性休克患者的相关因素,探讨判断疗效和预后的指标。方法 回顾性分析广东省老年医学研究所ICU 31例经血培养确诊念珠菌血症所致感染性休克患者(非中性粒细胞减少或缺乏)的临床资料,根据28天预后分为生存组和死亡组,观察两组患者第1、2、3、5和7天血降钙素原、C-反应蛋白、白细胞计数、血乳酸、序贯器官衰竭估计评分(SOFA)和急性生理与慢性健康状况系统Ⅱ评分(APACHE Ⅱ评分)等指标的动态变化,并对两组患者的相关资料进行统计学分析。结果 死亡组16例,生存组15例;血培养结果以非白色念珠菌居多(71%)、白色念珠菌占29%;两组患者第1天 APACHE Ⅱ评分和第1天血降钙素原差异有统计学意义。死亡组APACHE Ⅱ评分高于生存组[(27.63±5.14)vs. (22.60±5.88),P=0.017];生存组第1天血降钙素原[(2.74±2.32)ng/mL]较死亡组[(1.45±1.01)ng/mL]高(P=0.045);两组血降钙素原水平均随时间而变化 (P<0.05)且两组变化趋势的差异有统计学意义(P<0.05),变化曲线显示生存组第3天血降钙素原到达高峰[(4.27±5.19)ng/mL]、其后逐渐下降,而死亡组呈逐渐上升趋势(P=0.004)。Logistic回归分析显示,第1天血降钙素原和APACHE Ⅱ评分是影响28天预后的独立危险因素,分别为比值比=0.272(95%可信区间 0.084~0.883,P=0.030) 和比值比=1.349(95%可信区间1.052~1.731,P=0.018)。两组白细胞计数、C-反应蛋白、血乳酸和SOFA评分在各时间点的变化趋势差异无统计学意义。结论 老年念珠菌血症所致感染性休克患者(非中性粒细胞减少或缺乏),应早期选用覆盖非白色念珠菌的药物;血降钙素原水平和APACHE Ⅱ评分值是影响28天预后的独立危险因素;对相关指标的动态观察评估临床意义更大。
Objective To investigate related factors for prognosis in elderly critically ill patients with septic shock caused by candidemia.Methods Single center, retrospective and observational study, thirty-one non-neutropenic elderly septic shock patients caused by candidemia in intensive care unit (ICU) were enrolled. Levels of procalcitonin (PCT), C-reactive protein (CRP), white blood cell (WBC) count, blood lactic acid (LAC), sequential organ failure assessment (SOFA) score as well as acute physiology and chronic health evaluationⅡ (APACHEⅡ) score on 1st, 2nd, 3rd, 5th, 7th day after making a definite of diagnosis of septic shock caused by candidemia were collected. Patients were divided into survival group and death group according to 28-day mortality. Differences in parameters between two group were compared, and multiple logistic regression analysis was performed to identify the risk factors significantly associated with 28-day mortality.Results During the study period (January 2010 to December 2014), 31 septic shock patients caused by candidemia episodes in ICU were enrolled, of whom 71% were identified as non-albicans candida and 29% were candida albicans. There were 16 patients in death group and 15 patients in survival group. APACHEⅡscore in death group was significantly higher than those in survival group at first day[(27.63±5.14)vs. (22.60±5.88),P=0.017], and PCT in survival group was significantly higher than those in death group [(2.74±2.32) vs. (1.45±1.01),P=0.045]. PCT and APACHEⅡ score decreased in survival group with time dependency pattern after 3rd day. In addition, the results of effect analysis showed that there were significant differences in PCT and APACHEⅡ score between both groups (P<0.05). WBC, CRP, LAC, as well as SOFA score did not change significantly in both groups, and there were no significantly differences at each time point between both groups. Multivariable logistic regression analysis revealed that PCT (odds ratio 0.272, 95%CI 0.084~0.883, P=0.030) and APACHEⅡscore (odds ratio 1.349, 95%CI 1.052~1.731,P=0.018) were independently associated with 28-day mortality between two groups.Conclusion Antifungal agents sensitive to non-albicans candida should be a priority to those elderly non-neutropenic septic shock patients caused by candidemia in ICU; PCT and APACHEⅡscores are independently associated with 28-day mortality for those patients; and greater clinical significance could be attained with dynamic observation and evaluation of both parameters.
念珠菌血症(candidemia)的发病率和死亡率较高, 严重威胁生命[1, 2, 3]。念珠菌已经成为美国院内血流感染的第4位病原菌[4]。Chianscan研究显示, 中国重症患者侵袭性念珠菌感染的发病率为0.32%, 归因病死率为21.43%, 约95%的患者通过血培养结果确诊[5]。我国老年化的程度越来越高[6], 老年重症患者数量也逐渐增多。由于基础病多、多器官功能不全、各器官调节功能差、免疫功能受损和用药复杂等特点[7], 老年重症患者一旦罹患念珠菌血症并出现感染性休克, 将严重影响预后[8, 9, 10]。故探讨影响老年念珠菌血症的预后因素, 对及早采取干预措施、改善预后具有积极的临床意义。
本研究采用回顾性分析方法。2010-2014年广东省老年医学研究所重症医学科(intensive care unit, ICU)收治的休克患者, 入住后立即常规抽血做细菌培养。经血培养确诊为念珠菌感染性休克的患者(非中性粒细胞减少或缺乏)共31例; 其中男25例(80.6%), 女6例(19.4%); 年龄71~92(83.6± 5.8)岁, 其中> 80岁22例。感染性休克的诊断符合2012年严重脓毒症与感染性休克治疗国际指南的标准[11]。念珠菌菌株的分布为:白色念珠菌9例(29.0%); 非白色念珠菌22例(71.0%), 其中近平滑念珠菌12例(38.7%), 光滑念珠菌3例(9.7%), 热带念珠菌、无名念珠菌和罗伦隐球菌各2例(各占6.5%), 高里氏念珠菌1例(3.1%)。排除标准:年龄< 65岁; 入住ICU时间< 24小时; 晚期肿瘤以及粒细胞减少或缺乏患者。
收集所有患者的基线资料, 经血培养确诊念珠菌感染性休克的31例患者(非中性粒细胞减少或缺乏), 根据31例患者28天的预后分为生存组和死亡组, 分析比较两组患者第1、2、3、5、7天血白细胞计数(white blood count, WBC)、血降钙素原(procalcitonin, PCT)、C-反应蛋白(C reactive protein, CRP)、血乳酸(lactic acid, LAC)、序贯器官衰竭估计评分(sepsis-related organ failure assessment , SOFA)和急性生理与慢性健康状况系统Ⅱ 评分(acute physiology and chronic health evaluationⅡ score, APACHE Ⅱ 评分)等资料, 比较两组患者相关指标动态变化对预后的影响。其中WBC计数由血细胞分析仪检测; PCT 采用ELFA(酶联荧光分析)技术测定, 试剂购自BRAHMS (Di2 agnostica, Berlin, Germany) 公司, 按说明书进行操作; CRP的测定采用散射免疫比浊法, 参考值< 10 mg/L; LAC采用生化分析仪检测。
使用SPSS 19.0软件进行统计分析, 符合正态分布的计量资料用(均数± 标准差)表示并进行t检验, 计数资料用卡方检验或双侧Fisher精确概率法检验。应用重复测量方差分析和效应分析对各观察指标不同时点进行比较; 将单因素分析中差异有统计学意义的因素纳入Logistic回归模型进行多因素分析, 并进行生存分析。P< 0.05为差异有统计学意义。
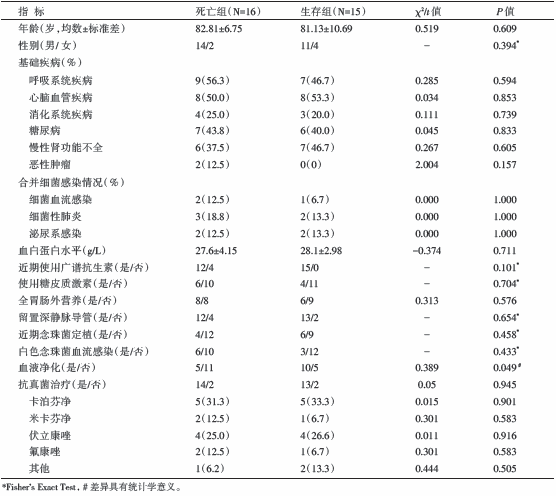
31例患者的28天死亡率为51.6% (16/31), 两组患者基线资料差异无统计学意义(P> 0.05), 生存组血液净化比例高于死亡组(66.7% vs. 31.2%, P=0.049), 见表1。
| 表1 两组患者基线资料比较 |
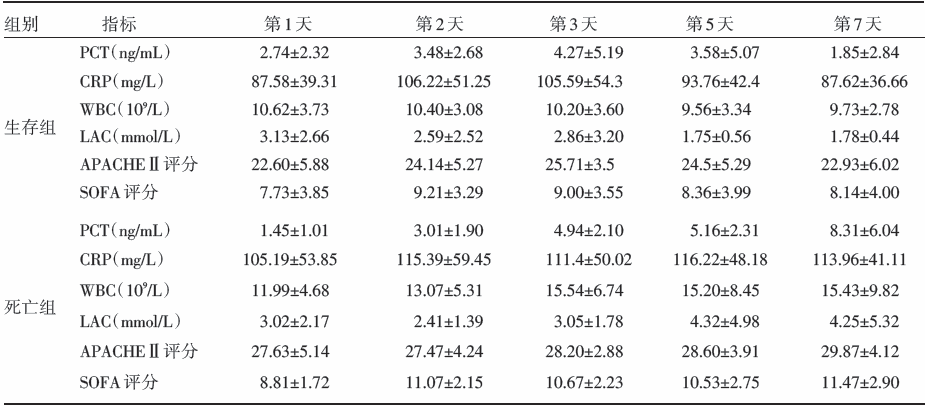
两组患者第1天 APACHE Ⅱ 评分、第1天 PCT水平差异有统计学意义, 死亡组APACHE Ⅱ 评分高于生存组[(27.63± 5.14)vs. (22.60± 5.88), P=0.017], 死亡组PCT低于生存组[(1.45± 1.01)ng/ml vs. (2.74± 2.32)ng/ml, P=0.045], 见表2; 随后各时间点上两组患者PCT值无显著性差异(P=0.145), 但两组PCT值均随时间变化(P=0.002), 生存组PCT 3天后随时间延长呈下降趋势, 死亡组呈上升趋势(P=0.004); APACHE Ⅱ 评分变化趋势类似PCT表现; 两组患者WBC、CRP、LAC和SOFA评分在各时间点变化趋势差异无统计学意义(P> 0.05)。见表3和图1。
| 表2 两组患者第1 天各观察指标比较 |
| 表3 死亡组与生存组患者不同时点指标比较 |
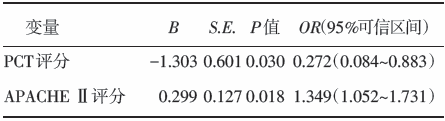
Logistic回归分析显示第1天 PCT和APACHE Ⅱ 评分是影响28天预后的独立危险因素, 分别为 比值比=0.272(95%可信区间0.084~0.883, P=0.030) 和比值比=1.349(95%可信区间 1.052~1.731, P=0.018), 见表4。
| 表4 Logistic 回归分析结果 |
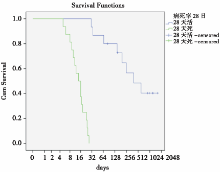
生存分析结果显示, 31名患者的平均生存时间为394天(95%可信区间163.81~624.47天), 中位生存时间27天(95%可信区间15.00~39.00天)。其中, 28天死亡组中位生存时间为14天(95%可信区间8.77~19.23天), 生存组平均生存时间为392天(95%可信区间0.00~985.55天), 两组生存时间存在差别(Log rank P< 0.001), 见图2。
ICU念珠菌血症发生率逐年上升[12], 粗死亡率高达35%~65%[13, 14, 15]。老年念珠菌血症患者进展至感染性休克阶段, 预后更差[16]。如何有效改善老年念珠菌血症所致感染性休克患者的预后是当今重症医学医师面临的重要课题。
既往研究认为[17, 18, 19, 20], 影响念珠菌血症患者预后的因素众多, 包括年龄、基础病情、诊断方法、治疗策略和致病菌种等。本研究以高龄患者(> 80岁)居多, 具有两种以上侵袭性念珠菌感染的危险因素和/或影响预后的不良因素, 这是31例患者28天死亡率高达51.6%的重要原因之一。既往文献报道中, 念珠菌血症的菌株主要以白色念珠菌居多[17, 18, 19, 20]。而本研究显示, 本组老年念珠菌血症的菌株主要为非白色念珠菌(71%)、其中近平滑念珠菌38.7%; 白色念珠菌仅占29%, 推测其原因与本组患者年龄大、反复住院、使用多种抗生素(包括抗真菌药物)等因素密切相关。因此, 老年念珠菌感染患者经验性抗真菌治疗的药物选择, 应详细评估既往诊治的情况, 早期选用覆盖非白色念珠菌的药物为佳。本研究基线资料显示, 两组患者抗真菌药物的选择并无显著性差异, 提示老年念珠菌血症患者的治疗涉及面广、复杂, 改善该类人群预后的措施或许是多方面措施综合作用的结果。另有文献报道, 血液净化是念珠菌血症预后不良的因素 [18]; 生存组血液净化的比例高于死亡组(66.7% vs. 31.2%, P=0.049); 我们推测这种差别与本研究的样本量较小、以液体和/或内环境平衡而非肾功能衰竭为血液净化时机等因素有关, 血液净化有利于维护内环境稳定、清除部分炎症介质、减轻炎症反应, 对改善预后可能有积极作用。
有研究报道[21], 单纯念珠菌血症患者PCT一般不超过5.5 ng/mL(阴性预测值100%, 阳性预测值65.2%), 本课题组前期的研究亦有类似结论[22]。本研究显示, 虽然两组患者PCT各个时间点的数值(除第1天外)无显著差异 (P> 0.05), 但生存组第1天 PCT值[(2.74± 2.32)ng/mL]较死亡组[(1.45± 1.01)ng/mL]高(P< 0.05); 两组PCT均随时间而变化 (P< 0.05)、且两组变化趋势存在显著差异 (P< 0.05), 变化曲线显示生存组第3天PCT值到达高峰(4.27± 5.19)ng/mL、其后逐渐下降, 而死亡组呈逐渐上升趋势; Logistic回归分析显示, 第1天 PCT是影响28天预后的独立危险因素(比值比为0.272)。另外, 本研究显示, 两组APACHE Ⅱ 评分各个时间点评分值的比较均存在显著差异, 死亡组较生存组高, 且两组随时间变化的趋势与PCT类似; 死亡组第1天 APACHE Ⅱ 评分较生存组高(P< 0.05), Logistic回归分析显示, 第1天 APACHE Ⅱ 评分是影响28天预后的另一独立危险因素(比值比为1.349)。故观察早期PCT和APACHEⅡ 评分、追踪其变化趋势, 对于判断老年念珠菌感染性休克患者的疗效和预后均具有重要临床意义。
本研究中, 两组患者的WBC、CRP、LAC和SOFA评分, 各时间点变化趋势的比较均未见显著差异, 可能由于本研究样本量小所致, 也可能表明这些指标对于判断老年念珠菌感染性休克患者疗效和预后的作用有限。
总之, 非中性粒细胞减少或缺乏的老年念珠菌血症所致感染性休克患者, 动态监测PCT和APACHE Ⅱ 评分及其变化趋势, 对疗效和预后的判断均具有重要意义, 二者结合临床应用价值更高。由于本研究为小样本回顾性研究, 相关指标及其相互间的临床意义, 有待今后积累更多资料进一步探索研究。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
|