作者简介:
李春林和黄津为共同第一作者。李春林(1985-),男,湖北来凤人,医学硕士,主治医师,主要从事介入放射学工作;黄津(1985-),女,湖北来凤人,医学学士,主治医师,主要从事妇产科相关工作。
目的 检索当前的最佳证据,为一例疑似免疫球蛋白G4(immunoglobulin G4,IgG4)相关性胰腺炎患者的进一步诊断与治疗提供最有力的证据。方法 计算机检索Embase数据库(1995-2019)、Medline数据库、Cochrane Library(Central数据库)(1995-2019)、UptoDate数据库、万方数据库(1995-2019)、中国知网CNKI(1995-2019)等,查找有关IgG4相关性胰腺炎的系统评价、临床指南、横断面研究、病案报道、文献综述、专家建议等,并对检索到的文献证据进行评价分级。结果 检索证据表明,局灶型IgG4相关性胰腺炎极易误诊为胰头癌,二者的鉴别有赖于胰腺穿刺活检;由于胰腺癌的治疗首选外科手术切除,而IgG4相关性胰腺炎首选糖皮质激素治疗,因此对胰腺癌患者的术前或疑似IgG4相关性胰腺炎患者进行胰腺穿刺活检显得尤为重要。结论 胰腺穿刺活检及血清免疫学检查对于诊断IgG4相关性胰腺炎的特异性和敏感性都比较高,糖皮质激素是治疗IgG4相关性胰腺炎的特异性药物。
Objective To search the best evidence so far, and to provide the most powerful evidence for the diagnosis and treatment of a suspected immunoglobulin G4-related autoimmune pancreatitis(IgG4-RAIP) in our hospital.Methods Searching for systematic evaluation, clinical guidelines, cross-sectional studies, medical record reports, literature review, expert recommendations, etc from Embase database (1995-2019), Medline database, Cochrane Library (Central database) (1995-2019), Uptodate database, Wanfang database (1995-2019), China knowledge net CNKI (1995-2019); evaluating and grading the literature evidences.Results The retrieved evidences show that focal IgG4-related pancreatitis is easily misdiagnosed as pancreatic head cancer, and the differentiation between them depends on pancreas biopsy. Since surgical resection is the first choice for the treatment of pancreatic cancer and glucocorticoid therapy is the first choice for IgG4-related pancreatitis, it is particularly important to perform pancreatic biopsy in patients with pancreatic cancer before operation or in patients with suspected IgG4-related pancreatitis.Conclusions Pancreas biopsy and serum immunological examination have high specificity and sensitivity in the diagnosis of IgG4-related pancreatitis. Glucocorticoid is a specific drug for the treatment of IgG4-related pancreatitis.
自身免疫性胰腺炎(autoimmune pancreatitis, AIP)由Yoshida等在1995年首次提出[1]。目前国际上公认将本病分为1型和2型两种亚型; 1型又称免疫球蛋白G4相关性胰腺炎(immunoglobulin G4-related autoimmune pancreatitis, IgG4-RAIP), 2型又称特发性导管中心性胰腺炎, 其中1型相对更加常见[2]。2011年日本学者Okazaki K等在《Clin Rev Allergy Immunol》发表的文献表明[3], 1型以血清IgG4升高为其临床特征, 常合并有胰腺外组织病变, 以50~70岁男性多见; 2型以胰腺组织粒细胞上皮损伤为其特征性表现, 血清IgG4一般不升高, 较少合并胰腺组织病变, 首次发病年龄通常较1型患者的年龄小。目前, IgG4-RAIP的病因与发病机制尚未被完全阐明[4, 5], 大多数学者认为本病是一种多因素、多机制共同参与的疾病, 其中以免疫机制占主导地位, 即由自身免疫机制所介导的, 以细胞质和淋巴细胞浸润为主的胰腺疾病, 常伴有胰腺纤维化及胰腺功能障碍, 是临床上比较少见的一类胰腺慢性炎症[6]。本病通常隐匿发病, 多数患者以无痛性梗阻性黄疸为首发症状, 约占75%[7], 部分患者可伴有中上腹部不适或轻中度疼痛, 影像学检查通常以胰腺局限性或弥漫性肿大为主, 因此常被误诊为胰腺癌, 误诊率高达56%[8, 9]。鉴于此, 我们结合本院具体病例, 以提出问题为基础, 以寻找证据为核心, 运用循证医学的基本原理和方法[10], 对IgG4-RAIP的诊断与治疗进行探索, 以供临床医师参考, 减少本病误诊误治的发生。
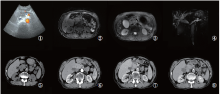
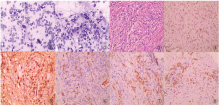
男性患者, 74岁, 因“ 发现胰腺肿物伴黄疸1月余” 入院。患者于2年前因上腹部疼痛在外院接受“ 胰腺炎” 治疗。出院后反复出现上腹部及剑突下疼痛, 行对症治疗效果不佳。1个月前再次出现上腹部疼痛, 在外院行对症治疗无好转, 症状逐渐加重遂来我院求诊, 我院门诊行上腹部CT检查提示胰腺肿物, 胆总管扩张。遂以“ 胰腺占位伴胆总管扩张” 收入外科, 拟行“ 胰腺肿瘤” 外科手术治疗。入院查血浆CA12-5、CA19-9、AFP、CEA值均正常。血浆D-二聚体升高(308 ng/mL), 血淀粉酶升高(283.5U/L), 黄疸指数(+)。彩超检查提示:胆囊肿大伴胆汁淤积, 肝内胆管及胰管扩张, 胰头区异常回声(占位性病变待排)(图1 ①)。MRI平扫显示:胰头区见结节状肿块, T1WI信号稍减低, T2WI信号稍减低(图1 ②~③); 磁共振胰胆管造影(magnetic resonance cholangio pancreatography, MRCP)提示胰头部肿块, 肿瘤性病变可能; 胰管、胆总管及肝内胆管扩张, 胆总管胰头部截断, 胆囊增大(图1 ④)。上腹部CT增强检查:胰头区见小片状稍低密度影, 边界不清, 动脉期病灶边缘强化, 静脉期及延迟期病灶逐渐呈充填式强化(图1 ⑤~⑧)。对上述各项影像学检查及生化指标进行综合分析, 初步诊断为胰头癌并梗阻性黄疸。故行经皮肝穿刺胆道引流术(percutaneous transhepatic cholangial drainage, PTCD)以缓解黄疸症状。鉴于目前缺乏病理学诊断依据, 对于胰腺癌的诊断尚缺乏最有力的证据, 决定行CT导向下胰腺穿刺活检术。活检细胞学HE染色显示:镜下见大量淋巴细胞及部分坏死细胞, 可见少量增大裸核(图2 ①~②)。病理检查提示:镜下见胰腺小叶间纤维组织增生伴大量慢性炎性细胞浸润, 以淋巴细胞、浆细胞为主, 小叶内少量慢性炎性细胞, 个别区域腺泡轻度增生, 未见其它特殊(图2 ③~④)。认为本例患者可疑诊断为IgG4-RAIP。
目前患者诊断尚未明确, 下一步治疗方案暂不能确定。决定对穿刺标本做免疫组化检查, 以指导进一步诊断与治疗。根据目前情况, 我们面临以下问题:
(1)IgG4-RAIP的诊断标准是什么?(2)胰腺穿刺活检免疫组化检查对于诊断IgG4-RAIP(包括类型)的价值如何?其敏感性和特异性如何?(3)是否还需要其它检查进一步佐证诊断?(4)若该患者确诊IgG4-RAIP, 我们将如何治疗?带着以上问题, 笔者检索了当前相关的临床研究证据, 试图运用循证医学方法来回答这一系列问题。
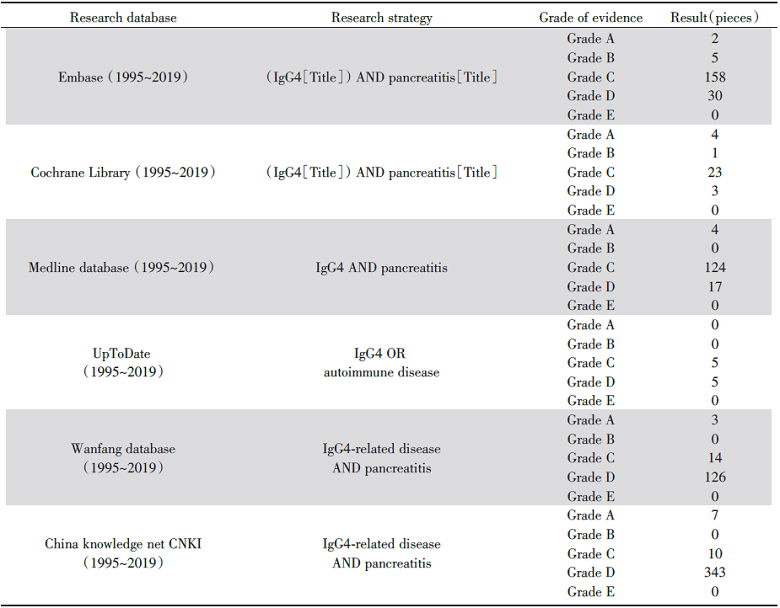
检索策略及检索结果见附表。根据2004年中国循证医学中心的证据级别五级分级法[11]将检索到的证据进行分级(见表1)。
| 表1 检索策略及检索结果 Tab.1 Search strategy and search results |
根据2011年国际胰腺病协会达成的共识, 对于可疑IgG4-RAIP患者, 病理学检查可以作为其诊断的“ 金标准” [2]。胰腺病灶靶向活检是鉴别胰腺癌与IgG4-RAIP必不可少的方法。我们通过Embase数据库检索到一项关于自身免疫性胰腺炎的组织病理学指南指出[12]:1型IgG4-RAIP病理学检查IgG4浆细胞数量明显增加, 通常每高倍镜视野> 50个; 而2型以粒细胞上皮病变为主要特征, 偶可见IgG4浆细胞, 且每高倍镜视野< 10个。在万方数据库中我们检索到一项对8例IgG4相关性疾病的临床和病理组织学研究指出[13], IgG4相关性疾病组织病理检查IgG4阳性的浆细胞每高倍镜视野为20~50个, 且IgG4/IgG> 40%。本例患者活检标本的免疫组化结果显示:浆细胞CD38、CD138、IgG阳性, IgG4部分阳性, 其中IgG4> 10/HPF, 且IgG4/IgG> 40%, Ki67低增殖(图2 ⑤~⑧)。查血清免疫球蛋白A及免疫球蛋白M均正常, 免疫球蛋白G升高(19.31 g/L), 抗核抗体(+)。血清IgG4检查结果为IgG4值13 g/L。验证了IgG4-RAIP诊断。回顾患者近两年来反复出现上腹部疼痛, 结合各项影像学检查、生化指标以及病理学检查结果, 可明确诊断为IgG4-RAIP, 硬化性胆管炎[2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14]。随后我们进一步在各大数据库中检索关于IgG4-RAIP治疗的证据。一项关于对IgG4-RAIP治疗的研究[15], 以及一项最新临床指南[16]均提示IgG4-RAIP治疗首选糖皮质激素, 并且疗效显著, 推荐起始治疗剂量为每日0.6 mg/kg, 2~4周后逐渐减量, 以2.5~5.0 mg/d的维持剂量治疗半年。遂给予本例患者口服泼尼松治疗, 起始剂量为40 mg/d。
患者口服糖皮质激素治疗4周后行CT平扫及MRI增强检查显示病灶明显缩小(图3), 血清IgG4检测值为1.2 g/L(参考值80~1 400 mg/L), 同时患者上腹部疼痛症状完全消失。
目前认为IgG4相关性疾病可累及人体所有器官, 既可表现为单个器官受累, 也可表现为多个器官同时受累[17], 胰腺是最常受累的器官之一[18]。IgG4-RAIP常伴有胰腺外其它器官受累, 以硬化性胆管炎及腹膜后纤维化最为常见[3]。2011年国际胰腺病协会经过多方面努力、研究及综合评估后制定了IgG4-RAIP的诊断标准, 包含5项基本指标:(1)胰腺实质或胰管的影像学改变; (2)血清IgG4的水平; (3)胰腺外其他器官受累情况; (4)胰腺组织的病理学表现; (5)对糖皮质激素治疗的敏感性[2]。IgG4-RAIP的影像表现大致可以分为三种类型, 即弥漫型、局灶型、多灶型[19]。其中以弥漫型最常见, 影像学检查表现为胰腺弥漫性肿大; CT平扫可显示病变区胰腺密度降低, MRI检查表现为病灶区T1WI信号减低, T2WI信号稍增高, 胰腺实质内部结构消失, 边缘比较清晰, 通常可见胰腺呈“ 腊肠样” 改变, 胰腺周围脂肪间隙清晰。CT或MRI增强检查病灶均表现为渐进性强化, 即病变区域动脉期呈轻度强化, 动脉期及延迟期病灶强化程度逐渐增加。约有36%的患者可表现出具有特征性的“ 晕环征” 。局限型多发生于胰头部, 超声检查表现为病灶区域回声减弱[20]; CT或MRI检查表现为局灶性低密度病变或T1WI信号减低, 胰腺局限性肿大, 病灶上游的胰管轻度扩张, MRCP检查显示肝内胆管扩张, 胆总管胰头部截断, 胰管扩张。因此极易与胰腺癌混淆[21]。一项国际多中心的相关研究表明[22], 内镜下逆行性胰胆管造影术(endoscopic retrograde cholangiopancreatography, ERCP)对于诊断IgG4-RAIP的敏感性及特异性分别为71%及83%。血清学检查方面, 血清IgG4增高是目前诊断IgG4-RAIP最有价值的指标[23], 且血清IgG4高于正常值2倍以上可显著增加诊断的准确性, 此时其敏感性和特异性分别为93%和99%; 部分患者可合并CA19-9轻度升高[24, 25]。根据国际胰腺学协会指南关于自身免疫性胰腺炎国际共识[2]及我国关于对IgG4相关疾病临床病理学特征的研究表明[13], IgG4-RAIP组织病理学改变有:(1)胰腺导管周围可见大量淋巴细胞、粒细胞及浆细胞浸润, 呈间质性炎症改变或小叶间纤维化改变; (2)IgG4阳性浆细胞数量> 10/HFP, IgG4/IgG> 40%; (3)胰腺实质呈席纹状纤维化改变; (4)闭塞性静脉炎症等。对该患者进行综合分析, 总结如下:(1)影像学检查, 彩超、CT及MRI均发现胰头区肿块伴胰管扩张; (2)血清IgG4为13 g/L, 高于正常值2倍以上; (3)MRCP显示胆囊增大, 肝内外胆管及胰管扩张; (4)病理学免疫组化:浆细胞CD38、CD138、IgG阳性, IgG4部分阳性, 其中IgG4> 10/HPF, 且IgG4/IgG> 40%; (5)患者口服糖皮质激素治疗4周后腹痛症状完全消失, CT平扫及MRI增强检查显示病灶明显缩小。该患者完全符合2011年国际胰腺病协会制定关于IgG4-RAIP诊断的上述5项基本指标[2]。
IgG4-RAIP治疗首选糖皮质激素。2012年Ebbo M等的一项多中心队列研究表明[26], 糖皮质激素治疗本病的敏感超过90%, 并且大部分患者经过2周激素治疗后临床症状可明显缓解, 影像学及血清学检查均可明显好转。目前国际上对该病使用糖皮质激素治疗的起始剂量和维持剂量尚未达成共识, 我国目前推荐口服泼尼松30 mg~40 mg/d或按0.6 mg/kg/d治疗2~4周后根据患者临床症状、影像学征象及血清学检查指标逐步减量, 以后以5 mg/d的维持剂量治疗半年以上, 经过半年的维持治疗后, 若患者临床症状消失, 影像学检查胰腺大小、形态正常, 血清学检查IgG4正常可作为停药指征[16]。
IgG4-RAIP因缺乏典型的临床症状和影像学表现, 临床上极易将本病误诊为急/慢性胰腺炎或胰腺癌, 从而导致延误治疗或错误的治疗, 甚至导致不必要的外科手术治疗。因此, 当临床遇到可疑IgG4-RAIP患者或者不能完全确诊的急/慢性胰腺炎、胰腺癌患者, 首先要完善影像学检查和血清学检查, 对于胰腺占位患者手术前应常规进行胰腺病灶靶向穿刺活检, 取出标本进行病理学、细胞学及免疫组化检查; 当不能完全确诊而又不具备完善上述检查时, 可以使用糖皮质激素进行诊断性治疗[27]。
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
|