作者简介:
荆文(1981-),男,山东高密人,主治医师,医学硕士,主要研究方向为泌尿系统恶性肿瘤外科治疗。
目的 探讨膀胱低度恶性潜能乳头状尿路上皮肿瘤(papillary urothelial neoplasm of low malignant potential,PUNLMP)患者经尿道膀胱肿瘤电切术(transurethral resection of bladder tumor,TURBT)预后的影响因素。方法 回顾性分析邯郸市第一医院2013年1月至2019年12月收治接受TURBT术治疗的膀胱PUNLMP患者共170例,单因素和多因素logistic回归分析患者TURBT术预后的影响因素。结果 术后随访6.5~92.0个月,中位随访时间27.0个月,无肿瘤相关性死亡事件发生。42例肿瘤复发,复发时间2.5~87.5个月,中位复发时间24.0个月。24例进展,进展时间3.0~58.0个月,中位进展时间为23.5个月。单因素分析结果表明初发肿瘤最大径和数量与TURBT术后复发和进展有关。多因素logistic回归分析结果显示,初发肿瘤数量是PUNLMP患者TURBT术后复发和进展的独立影响因素( P<0.05)。结论 初发肿瘤数量与膀胱PUNLMP患者TURBT术的预后密切相关;术后膀胱灌注化疗无法改善此类患者临床预后。
Objective To investigate the influencing factors of clinical prognosis in patients with papillary urothelial neoplasm of low malignant potential (PUNLMP) after transurethral resection of bladder tumor (TURBT).Methods Clinical data of 170 patients with low malignant potential bladder PUN after TURBT were retrospectively chosen from January 2013 to December 2019 in The First Hospital of Handan City. Univariate and multivariate methods were used to evaluate the influencing factors of clinical prognosis after TURBT.Results The patients were followed up for 6.5 to 92.0 months with a median time of 27.0 months and no tumor-related death occurred. 42 patients had tumor recurrence, the recurrence time was 2.5~87.5 months, and the median recurrence time was 24.0 months. 24 cases with progression, with the median progression time of 23.5 months ranging from 3.0 to 58.0 months. Univariate analysis showed that the maximum diameter and number of primary tumors were related to the recurrence and progression after TURBT. Multivariate analysis showed that the number of primary tumors was the independent factor affecting the recurrence and progression of bladder PUN patients with low malignant potential after TURBT ( P<0.05).Conclusions The number of primary tumors is closely related to the clinical prognosis of bladder PUN patients with low malignant potential after TURBT and postoperative intravesical chemotherapy should not improve the clinical prognosis of patients.
既往研究表明目前膀胱癌发病率高居泌尿系肿瘤第2位, 且发病率和发病人数均呈逐年增高趋势[1]。国际泌尿病理协会(International Society of Urological Pathology, ISUP)和世界卫生组织(World Health Organization, WHO)于1998年首次提出低度恶性潜能乳头状尿路上皮肿瘤(papillary urothelial neoplasms of low malignant potential, PUNLMP)这一概念, 认为其生物学侵袭性介于乳头状瘤和癌间, 2004年WHO/ISUP正式将这一类型列入非浸润性乳头状移行细胞肿瘤[2]。近年国内外对膀胱PUNLMP的报道逐渐增多, 但对于经尿道膀胱肿瘤电切术(transurethral resection of bladder tumor, TURBT)后复发或进展影响因素尚存争议[3]。本研究回顾性分析了邯郸市第一医院泌尿二科2013年1月至2019年12月接受TURBT术治疗的170例PUNLMP患者, 旨在探讨膀胱PUNLMP患者TURBT术预后的影响因素。
回顾性分析PUNLMP患者170例, 男性128例, 女性42例, 年龄21~87岁, 平均年龄(57.82± 6.44)岁。均为初次诊断, 接受TURBT术治疗, 经病理组织学确诊为膀胱非浸润性乳头状移行细胞肿瘤, 亚型确认为PUN, 同时排除远处转移。全部患者均由两名副主任及以上职称病理医师参考WHO泌尿系统和男性生殖器官肿瘤(2016版)标准完成诊断。
查阅患者病例, 记录年龄、性别、吸烟史、肿瘤最大径、肿瘤数量及伴内翻生长情况等, 其中多发肿瘤中选择最大肿瘤的最大径作为多发肿瘤最大径。采用住院复查方式完成随访; 术后前24个月内每3个月随访1次, 之后每6~12个月随访1次; 随访截止时间为2020年9月。术后复发指TURBT术后膀胱内再次出现PUNLMP, 术后进展指TURBT术后膀胱内再次出现低级别/高级别乳头状尿路上皮癌、原位癌其他膀胱恶性肿瘤类型[4]。根据患者意愿给予术后膀胱灌注治疗, 具体方案如下:丝裂霉素20 mg, 表柔比星50 mg, 吉西他滨1 000 mg, 吡柔比星50 mg; 术后24 h内开始首次灌注, 每周1次, 连续6次。
采用SPSS 22.0统计软件对数据进行分析。计量资料用均数 ± 标准差(x ± s)表示, 组间比较采用t检验。计数资料用例数(百分率)表示, 组间比较用χ 2检验。单因素和多因素logistic回归分析预后影响因素。P< 0.05为差异有统计学意义。
170例患者中因肉眼血尿就诊94例, 体检发现71例, 因下尿路刺激症状就诊5例。单发肿瘤122例, 其中膀胱侧壁68例, 输尿管口旁30例, 三角区14例, 后壁6例, 顶壁4例。多发肿瘤48例, 其中19例2个肿瘤, 29例≥ 3个肿瘤, 均分布于膀胱左右侧壁和输尿管口周围区域。
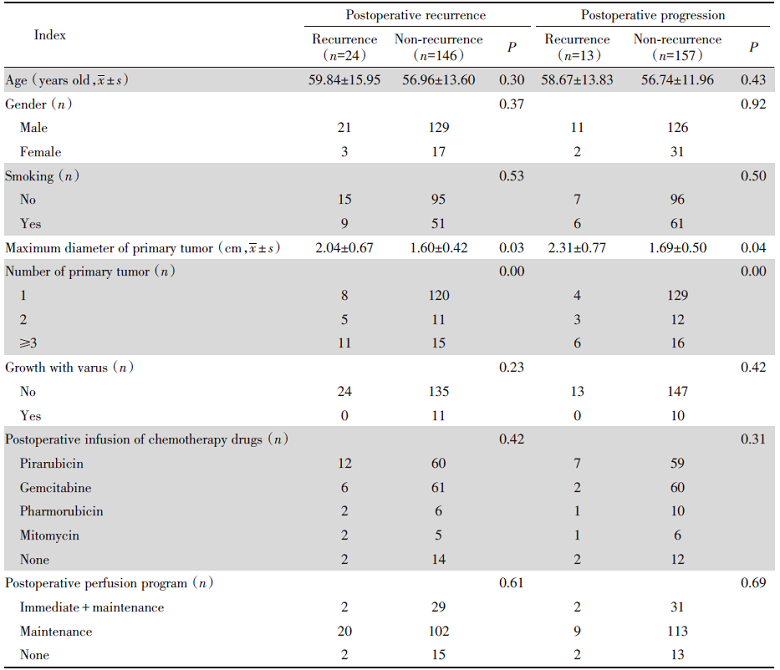
术后随访6.5~92.0个月, 中位随访时间27.0个月, 无肿瘤相关性死亡事件发生。42例肿瘤复发, 复发时间2.5~87.5个月, 中位复发时间24.0个月。24例复发患者中出现进展13例, 其中11例低级别/高级别非浸润性乳头状尿路上皮癌, 1例高级别浸润性尿路上皮癌, 1例鳞癌。进展时间3.0~58.0个月, 中位进展时间为23.5个月。单因素分析结果表明初发肿瘤最大径和数量与TURBT术后复发和进展有关(P< 0.05), 见表1。
| 表1 TURBT术后复发和进展影响因素的单因素分析 Tab.1 Univariate analysis of factors influencing postoperative recurrence and progression of TURBT |
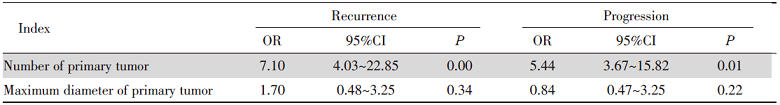
多因素logistic回归分析结果显示, 初发肿瘤数量是PUNLMP患者TURBT术后复发和进展的独立影响因素(P< 0.05); 但初发肿瘤最大径并非是PUNLMP患者TURBT术后复发和进展的独立影响因素(P> 0.05), 见表2。
| 表2 多因素logistic回归分析TURBT术后复发和进展影响因素 Tab.2 Multivariate logistic regression analysis of factors influencing postoperative recurrence and progression of TURBT |
2004年WHO/ISUP组织将PUNLMP正式列为单独类型, 目前认为其属于交界性肿瘤, 恶性程度介于乳头状瘤和低级别尿路上皮癌, 生物学侵袭性仍有待进一步探索[5]。考虑到膀胱PUNLMP术后复发较高, 但进展比例相对较低, 以往研究多将其纳入非浸润性乳头状移行细胞肿瘤进行分析[6]。
本研究纳入患者均为初诊膀胱PUNLMP患者, 严格排除复发、低级别乳头状尿路上皮癌或其他更高级别恶性肿瘤。以往报道认为初诊低级别乳头状尿路上皮癌治疗后复发者远期复发进展风险较高[7]。本研究结果表明76%单发肿瘤位于膀胱侧壁和输尿管口周围, 且男性发病率更高, 与既往报道结果相符[8]。另一项针对膀胱癌患者的meta分析结果证实[9], 非肌层浸润性膀胱癌(non-muscle invasive bladder cancer, NMIBC)吸烟人群局部复发风险较非吸烟人群更高, 但并未对PUNLMP患者分层分析。合并吸烟史并未对患者TURBT术后复发和进展产生影响; 但初发肿瘤数量被证实与患者TURBT术后复发和进展独立相关, 其中多发肿瘤人群术后肿瘤复发和进展比例更高。
有学者针对单纯接受TURBT术和术后行膀胱内灌注化疗辅助进行比较, 结果显示术后膀胱内灌注化疗有助于降低术后复发风险[10]。但本研究结果显示, 术后是否接受膀胱灌注化疗并不影响患者预后。此外不同膀胱化疗方案亚组术后复发和进展率比较差异亦无统计学意义, 故对TURBT术后膀胱灌注化疗应用价值仍有待进一步探索。
本研究11例患者存在内翻性生长, 其中3例肿瘤最大径> 3 cm多发肿瘤, 以上患者随访过程中均未见复发。已有研究显示[11], 尿路上皮肿瘤结构多呈外生乳头状, 但亦有部分呈内生生长, 可见于乳头状瘤、PUNLMP、低/高级别尿路上皮癌等。一项针对低级别非浸润性尿路上皮癌患者的临床病理资料分析显示, 存在完全或部分内生生长患者的术后复发率为38%, 远低于外生生长人群, 同时术后首次复发时间更长, 复发频率更低; 此外存在内生生长患者80%以上未见复发[12, 13]。本研究中伴内翻生长患者未表现出无复发优势, 笔者认为这可能与纳入样本量较少、随访时间短有关, 后续仍需更大样本、更长随访研究确证。
综上所述, 初发肿瘤数量与PUNLMP患者TURBT术后临床预后密切相关, 术后膀胱灌注化疗无法改善此类患者临床预后。
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|